Potential mechanical triggers behind inherited heart disease focus of new study
Nathaniel Huebsch receives nearly $2 million NIH grant

Hypertrophic cardiomyopathy is the most common cause of sudden death in young people. The genetically inherited condition causes the heart muscle to enlarge, making it difficult for the muscle to relax between beats and often creating an irregular heartbeat. Hypertrophic cardiomyopathy is caused by genetic mutations in the sarcomere, a protein apparatus that cardiomyocytes use to contract as the heart pumps blood. However, not all individuals with sarcomere mutations develop hypertrophic cardiomyopathy, even if they harbor similar mutations. This suggests that non-genetic factors may trigger the disease in patients who have genetic mutations.
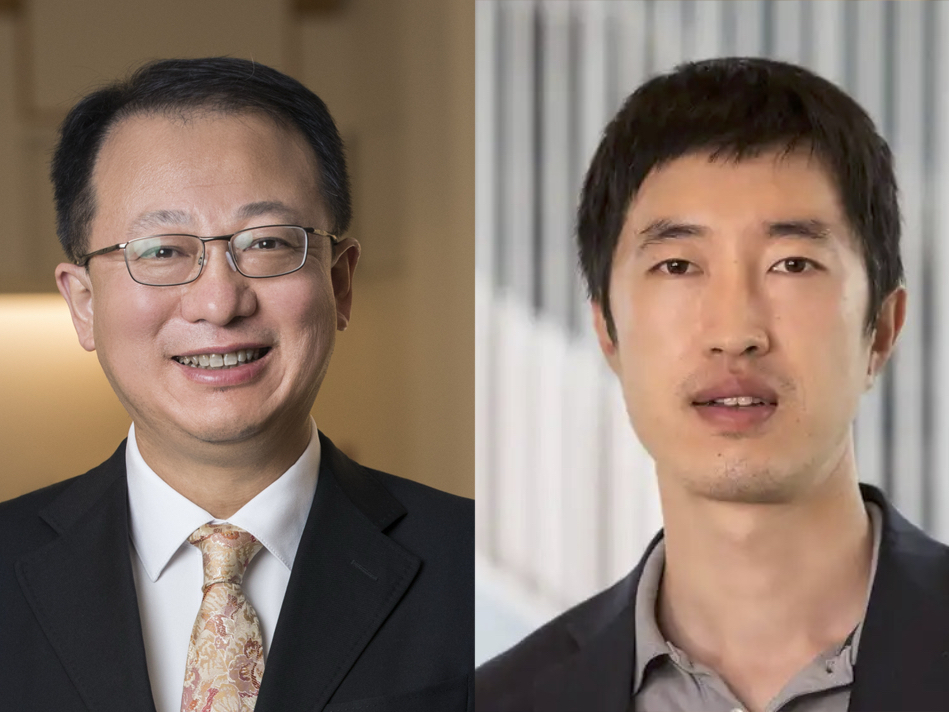
Nathaniel Huebsch, assistant professor of biomedical engineering in the McKelvey School of Engineering at Washington University in St. Louis, will research the role that blood pressure plays in triggering symptoms in patients with hypertrophic cardiomyopathy with a five-year, nearly $2 million grant from the National Institutes of Health. He and his team will use a heart tissue model engineered from human induced pluripotent stem cells (iPSCs) to identify molecular mechanisms that sensitize heart muscle to the mechanical load imparted by hypertension.
Hypertrophic cardiomyopathy is linked to several proteins in the sarcomere, but myosin binding protein C is the most prevalent protein with mutations in patients with this disease. Huebsch, whose expertise is in basic and translational stem-cell mechanobiology, seeks to elucidate the mechanism by which mechanical stress caused by high blood pressure advances the disease state. This knowledge may lead to new, more effective treatments for the condition.
“One of the interesting things we’re trying to understand is that people without sarcomere mutations who also have high blood pressure also show pathological enlargement of the heart muscle. The difference is that in patients without sarcomere mutations, the remodeling can be reversed with medications that reduce blood pressure,” Huebsch said. “However, in patients with hypertrophic cardiomyopathy, it is unclear whether these blood pressure medications have the same effect.”
Part of the work ahead will be to analyze the physiology of the disease to determine whether it is reversible and to understand the molecular pathways triggered as the disease progresses. Huebsch and his team plan to use iPSCs to create a “heart in a dish,” using cells engineered to harbor mutations in MYBPC3 at the Genome Engineering & iPSC Center at Washington University School of Medicine.
“The Huebsch lab’s heart in a dish system offers unique potential to uncover the critical mechanobiology of this epigenetic pathology,” said Guy Genin, the Harold and Kathleen Faught Professor of Mechanical Engineering, a collaborator on this grant. “Nate’s innovations add a powerful new toolset to link theory to experiment that has implications far beyond this specific disease.”
Ultimately, Huebsch and his lab expect to determine how mechanical stress and genetic mutations combine to make patients vulnerable to developing hypertrophic cardiomyopathy. Their understanding of the molecular pathways responsible for disease progression could enable more effective treatment options for patients suffering from the disease.