Mechanical causes behind congenital heart defect under new focus
Work in Jessica Wagenseil’s lab targets new drug strategies
Mutations in the elastin gene are believed to be behind supravalvular aortic stenosis (SVAS), a genetic defect that causes narrowing of the aorta, thus increasing the risk of sudden cardiac death. But there may be an additional contributor to this rare genetic disorder, for which there is no pharmaceutical treatment.
Jessica Wagenseil, professor of mechanical engineering & materials science in the McKelvey School of Engineering at Washington University in St. Louis, plans to look at the role of altered mechanics on smooth muscle cells in the aortic wall with a four-year, $1.6 million grant from the National Institutes of Health. Results of this work may help to identify new drug strategies that could prevent some of these changes.
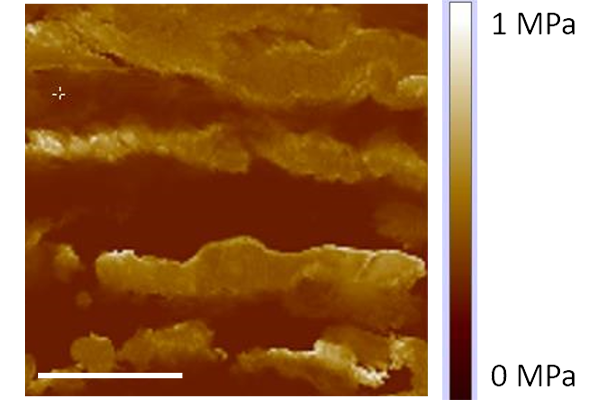
Wagenseil, also vice dean for faculty advancement, has long studied elastin, a protein that is a key component of a network of elastic fibers that allows the aorta to expand and contract in response to mechanical strain, such as blood pressure. Building on that work, she and her lab will look at changes in the way smooth muscle cells convert a mechanical stimulus, such as strain, if there has not been enough elastin laid down during development needed to stiffen the aortic wall.
“We hypothesize that increased strain on the smooth muscle cells causes activation or overexpression of the protein Piezo2, which leads to downstream signaling events that contribute to stenosis,” Wagenseil said.
Wagenseil and her team will test their theory in a mouse model and in human smooth muscle cells taken from patients with SVAS. They will look at strain under different conditions at various points in development, measure Piezo2 activity in mouse and human smooth muscle cells under strain and manipulate genetic activity in mouse aorta and mouse and human smooth muscle cells to determine its effects on the severity of stenosis.