Skin pigmentation bias in pulse oximeters to get closer look
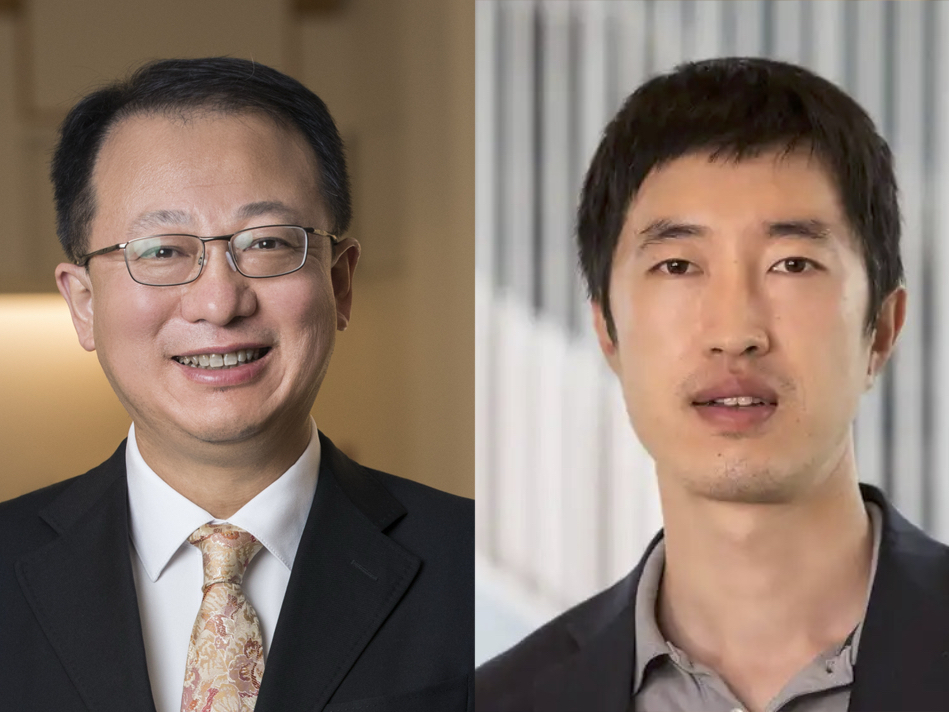
Christine O’Brien, Leo Shmuylovich, MD, PhD, seek to overcome bias that impacts marginalized community

Pulse oximeters send light through a clip attached to a finger to measure oxygen levels in the blood noninvasively. Although the technology has been used for decades — and was heavily used during the COVID-19 pandemic — there is increasing evidence that it has a major flaw: it may provide inaccurate readings in individuals with more melanin pigment in their skin. The problem is so pervasive that the U.S. Food & Drug Administration recently met to find new ways to better evaluate the accuracy and performance of the devices in patients with more pigmented skin.
Christine O’Brien, assistant professor of biomedical engineering in the McKelvey School of Engineering and of obstetrics & gynecology in the School of Medicine, and Leo Shmuylovich, MD, PhD, assistant professor of medicine in the Department of Dermatology at the School of Medicine, both at Washington University in St. Louis, are seeking ways to mitigate this potential bias. With a two-year, $375,000 grant from the National Institutes of Health’s National Institute of Biomedical Imaging and Bioengineering, O’Brien and Shmuylovich are looking at using new experimental systems that allow skin pigmentation to be varied while all the other physiologic parameters remain the same as well as changing the pulse oximeter wavelengths from red light to short-wave infrared light, which minimizes melanin absorption and scattering.
“The racial bias observed from in these devices may cause harm by impeding respiratory support in individuals with low blood oxygenation,” O’Brien said. “Overcoming this bias and separating it from other sources of potential error in the oximeter is critically important to ensuring that patients with more pigmented skin are not denied lifesaving care due to devices that fail to meet the needs of a diverse population.”
Pulse oximeters detect how tissue absorbs red and infrared LEDs, and oxyhemoglobin and deoxyghemoglobin absorb the lights differently. Researchers think that differences in melanin-related absorption and scattering of the light, particularly at red wavelengths, is behind the pigmentation-related errors in estimating oxygenation and may also impact estimates of the way blood flows through the circulatory system to an organ or tissue. However, previous studies looking at these errors have not controlled for other physiologic factors that may impact pulse oximetry, so it is unknown whether the health disparities that those with pigmented skin face may drive these errors.
Joining the team is Mitchell Pet, MD, associate professor of surgery (plastic & reconstructive surgery), who developed the preclinical model with Shmuylovich that allows researchers to simultaneously make measurements on different areas of pigmentation to check if a given device has pigment sensitivity.
“We expect at the end of our research, this lifesaving pulse oximeter technology serves the needs of patients independent of their pigmentation and no longer fails an already marginalized community,” Shmuyolovich said.