Before test results, signs of COVID-19 are in water systems
A meta-analysis helps epidemiologists, engineers talk to each other

Before a community hospital is stretched thin with COVID-19-patients, even before antigen tests — no matter how rapid — return results, there is one place that may be able to capture the number of COVID-19 infections in a community.
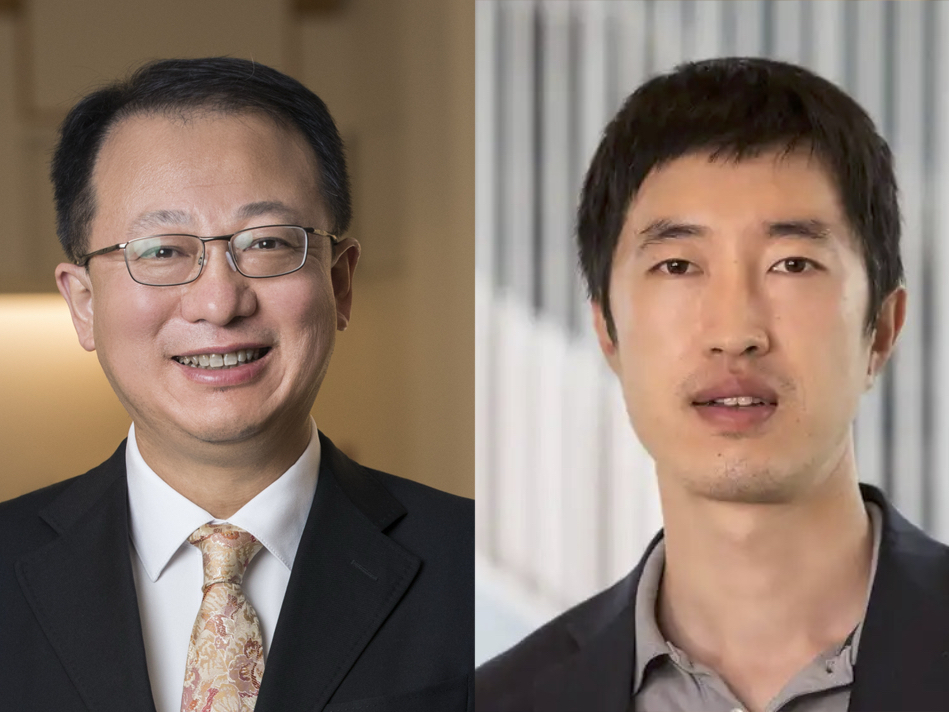
A new research paper from the lab of Fangqiong Ling, assistant professor of energy, environmental and chemical engineering at Washington University in St. Louis’ McKelvey School of Engineering, has shown the viability of wastewater as an accurate tool when it comes to describing COVID-19 outbreaks in a community. Beyond proving the usefulness of COVID-19 detection, the breadth of the paper’s analysis also makes it a resource for other researchers in the fast-growing field of wastewater epidemiology.
The research was published as the cover story of the July 22 issue of the journal Environmental Science, Water Research & Technology.
Since the beginning of the COVID-19 pandemic, researchers across the world have begun or ramped up existing water monitoring programs. Working collaboratively with the Washington University School of Medicine and researchers from two other universities, Ling and David Mantilla-Calderon, a postdoctoral associate in her lab, took advantage of the data to determine what, if any, relationship they could find between the number of COVID-19 cases reported in an area and the amount of genetic material from SARS-CoV-2 in municipal wastewater.
Starting with 101 studies of wastewater from around the globe, Ling and her team decided on a set of common variables and other inclusion criteria that had to be met to accurately combine data for a kind of “study of studies” known as a meta-analysis systematic review. This kind of study allows researchers to investigate a question using much more data than they could have collected themselves; ultimately, they were able to use 20 of the 101 studies.
“In general, we found a positive correlation,” Mantilla-Calderon said. As recorded cases went up, they found more viral material in the wastewater. “But it’s not a one-to-one correlation — the strength of the correlation changes with each system.” That’s because every wastewater system is unique. Mantilla-Calderon knows this better than most because he has a background in wastewater monitoring and is familiar with the ways these systems can vary.
Wastewater systems can be built from different materials and use different processes or chemicals at different parts of the system. They often are built in different configurations and serve vastly different-sized populations. Adding to the study’s complexity, among the 20 papers that shared enough variables to be included in the study, different researchers used different RNA extraction methods.
It’s these quirks of individual wastewater systems and of researchers’ methods and preferences that have led to a field full of data without enough context to make it generalizable. With this paper, however, Ling’s lab has made a significant contribution toward defining that context.
“The study provides general statistical guidance,” Mantilla-Calderon said. In the future, researchers will be able to use it to help them better understand how to interpret their data, given the kinds of samples they have and the systems they are working with.
It also begins to bridge any gaps between medical researchers and engineers.
“We use the same kind of meta-analysis systematic review method that’s typically used in clinical research,” Ling said. “This creates a kind of common language for medical researchers and engineering researchers.”
This may facilitate the exchange of data and results, leading to a more robust understanding of the relationships between viruses moving through the engineered world and diseases spreading through populations.
This work is supported by a National Science Foundation CAREER Award (no. 2047470) and the Washington University Faculty Startup Fund.