Spongy electrodes designed for better births
New technology should help doctors learn more about preterm labor, while making it easier on patients

In nearly 10% of pregnancies worldwide, birth comes early. Far from being a pleasant surprise, preterm births increase the likelihood of complications ranging from anemia and jaundice to cerebral palsy and learning disabilities.
Despite its well-known risks, doctors are still working to understand why some people go into labor early. The current technology used to map uterine contractions with the sensitivity needed to create a 3D visualization is too cumbersome to be used with any regularity; it’s reserved for clinical trials but wouldn’t be feasible for the average patient.
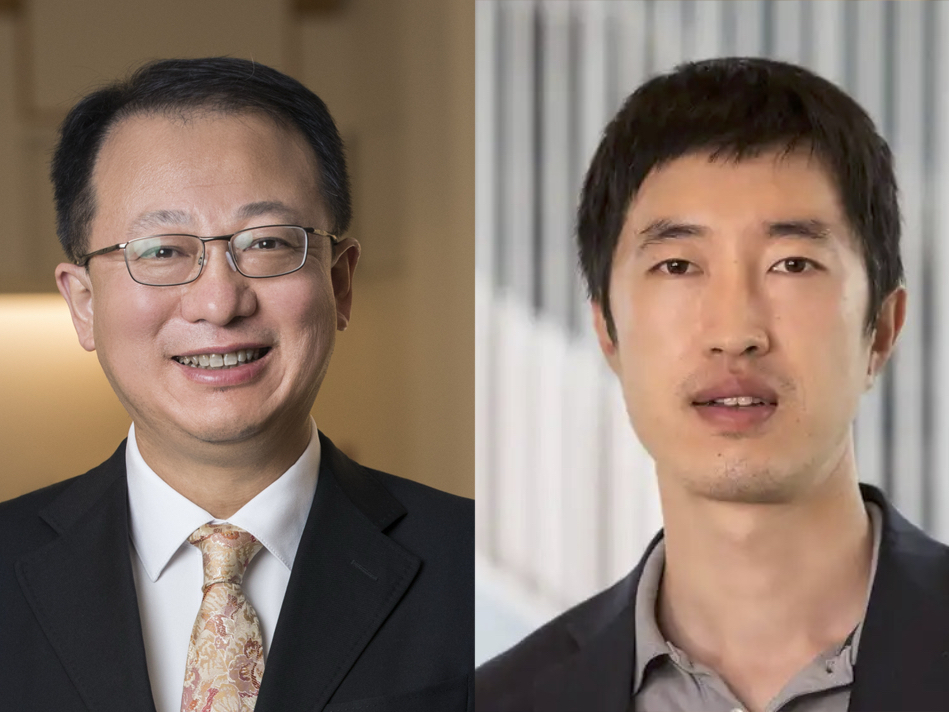
Enter the labs of Chuan Wang, assistant professor; Shantanu Chakrabartty, the Clifford W. Murphy Professor; and Yong Wang, associate professor, all in the Preston M. Green Department of Electrical & Systems Engineering at the McKelvey School of Engineering at Washington University in St. Louis. Yong Wang also has an appointment in the departments of Obstetrics & Gynecology and Radiology at the School of Medicine. The team has developed a technology that may help doctors collect the data they need without the patient needing to leave home.
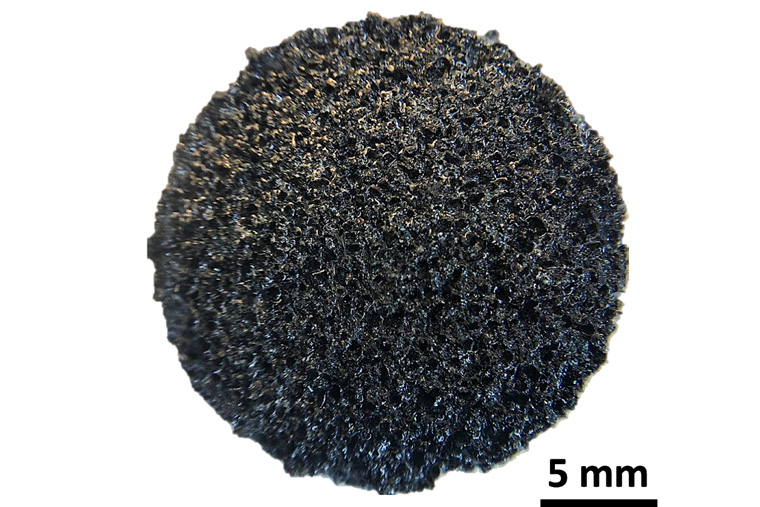
The details of the soft, sponge-like electrodes the team developed were published July 21 in the journal ACS Nano.
“The current technology is great, but it is very cumbersome to apply hundreds of wired electrodes to a patient, especially in the later stages of pregnancy,” Chuan Wang said. “Patients have to sit still, and it takes sometimes a half hour just to apply the electrodes.”
Wang’s new technology involves ultrathin, spongy electrodes — made from a conductive polymer — that can collect high-quality electrophysiologic signals from the body in less time and without the need for a trip to the hospital.
There are several major benefits to using a spongy material for electrodes: It is soft and stretchable, much more comfortable and there is no tangle of wires. “Ideally, we’d like to use it in a textile, or smart clothing,” Wang said.
Like dishwashing detergent in a sponge, a conductive gel fills the spongy material’s micropores. An electrode in use today collects signals from the area where the electrode is attached to the skin; in contrast, the pores of a spongy electrode hold gel, which means the inner surface of all the micropores are in electrical contact with the skin. “Effectively, we are increasing the electrode surface area by five times while not occupying any more space.”
This means the electrode can record cleaner electrocardiogram (ECG) or electromyogram (EMG) signals with better signal-to-noise ratio from the body.
Gel-filled pores also make good shock absorbers and help reduce motion-artifacts. In a hospital setting, any sudden movement — sitting up, for example — can lead to a loss of signal. Wang’s sponge, however, deforms and moves with a person. In experimental settings, the soft electrode was able to continue capturing ECG signals that conventional electrode missed when the subject was in motion.
And the electrode can capture data over many hours, whereas a traditional electrode cannot, because of the increased staying power of the conductive gel, trapped inside the spongy electrode’s pores.
“It’s similar to a dish sponge — soak it in water and it takes a very long time to dry.
“For a conventional electrode, after about an hour, the gel dries and the signal is gone,” but after three hours, the sponge electrode’s signal has barely lost strength.
Wang’s lab recently received a grant for the next phase of the project — powering the electrodes wirelessly so the patient can collect and transmit data without leaving home.
This work was funded by the Bill & Melinda Gates Foundation (INV-005417, INV-035476)