Portable, low-cost tech tracks uterine contractions
Detecting preterm birth could lower mortality

Keeping track of pregnancy requires a dizzying array of gargantuan and expensive machines. An MRI machine is the size of a room and can cost up to $1 million. But the care such equipment provides is a critical part of prenatal care, especially for dealing with complications like preterm birth. To get this care, pregnant people frequently need to visit a hospital, a significant burden for underserved and disadvantaged communities.
In a paper published May 19 in early access online in IEEE Transactions on Biomedical Circuits and Systems, a collaboration of researchers at Washington University St. Louis described a more accessible route to care: a portable uterine-contraction tracker, a cheap-to-make, flexible electrode patch.
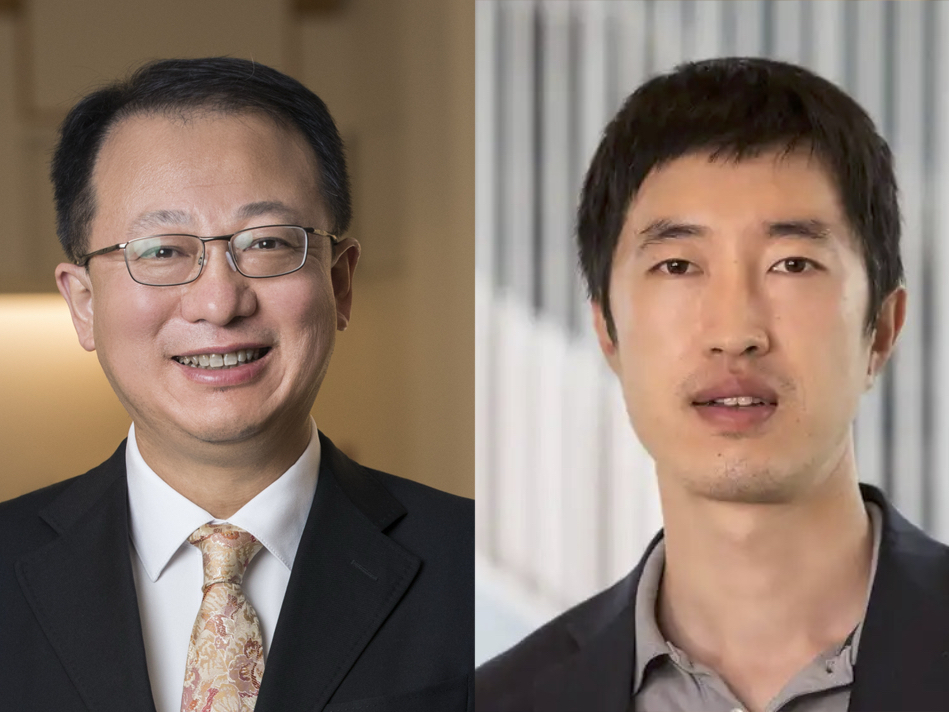
The paper builds on previous work from Washington University researchers. In 2019, Yong Wang, associate professor of obstetrics and gynecology at the School of Medicine, published a paper describing the creation of noninvasive electromyometrial imaging (EMMI). This method monitors electrical signals generated by uterine contractions and can detect unusual and preterm contraction patterns. Shantanu Chakrabartty, the Clifford W. Murphy Professor in the McKelvey School of Engineering, and Chuan Wang, associate professor of electrical & systems engineering in the McKelvey School of Engineering, led an effort to shrink down that technique invented by Wang, who was also a collaborator on this new work. Weilun Li, a doctoral student in Chakrabartty’s lab, is the first author on the paper.
Preterm birth, birth before 37 weeks of gestation, is one of the biggest causes of maternal and fetal mortality in the United States. According to the World Health Organization, there are about 13.4 million preterm births worldwide, a rate of more than one in 10 births. The burden of mortality is not evenly distributed. More than 90% of extremely preterm babies, delivered before 28 weeks, born in low-income countries will die, where less than 10% of extremely preterm babies born in high-income countries will die. Babies born preterm can develop a variety of breathing and bleeding problems and require rapid NICU treatment.
The current systems used by Yong Wang’s group for EMMI imaging are bulky, large, complex and costly. The system costs more than $20,000, and patients must visit his lab to use the equipment.
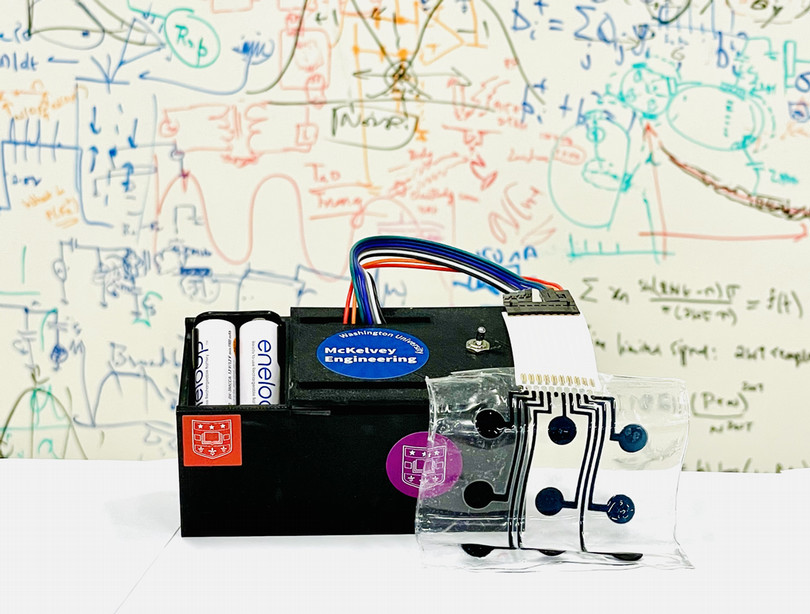
To get the same information that the bulky EMMI system provides, Chakrabartty’s lab created a battery-powered portable instrumentation that connects with a stretchy patch that places electrodes around the wearer’s abdomen. The electrodes detect both maternal heartbeat and EMG signals, which correspond to uterine contractions. Chuan Wang created flexible electrodes that Chakrabartty’s group used to build the device.
The new, portable EMMI can both store the pattern of contractions itself and transmit the data wirelessly to a computer for analysis. The materials used in the portable device, and flexible electrodes created with a low-cost inkjet printing process, along with commercially available, off-the-shelf chips, cost about $200.
To check the accuracy of the portable EMMI, the researchers tested it on low-risk term labor patients scheduled to be induced at the Washington University Medical Center. They compared the EMMI’s readings with the current gold standard measurement, a tocodynamometer, or TOCO for short. TOCO measures the mechanical pressure created by uterine contractions. Through a filtering algorithm, the researchers reduced noise and artifacts often introduced when a patient moves around, either in their daily lives or in a medical setting like an ambulance. The electronic signals EMMI captured lined up precisely with TOCO measurements, which is especially impressive given that EMG signals are “quite feeble,” on the order of 100 microvolts or less, according to Chakrabartty.
The portable EMMI is a proof of concept, showing that they could create an eight-channel battery-powered device to detect contractions and maternal heartbeats. The goal for future research is to scale up to 256 channels to produce crisper data. Because of the off-the-shelf textiles and chips, “you can just add more electrodes and channels, there’s no need to redesign the whole thing as you scale up,” Chakrabartty said.
“The novel wearable EMMI system has brought about a remarkable enhancement in patient accessibility, revolutionizing the way we monitor and care for individuals,” said Yong Wang. “Building upon this groundbreaking advancement, we are now preparing to embark on multi-site clinical trials focusing on several obstetric conditions with NIH and Gates Foundation. This exciting endeavor will allow us to gather comprehensive data and further advance our understanding and treatment of these conditions.”
As production scales up, the cost of production should drop below $200. The research was funded by the Bill and Melinda Gates Foundation, which intends to commercialize the technology and distribute it in low-income countries.
Chakrabartty said he envisions a future where a pregnant person could wear a portable EMMI most of the day in their own homes. It would wirelessly transmit continuous data to their doctor’s office, who would immediately be aware of any concerning changes in the pregnancy without the need to have patients come in person.
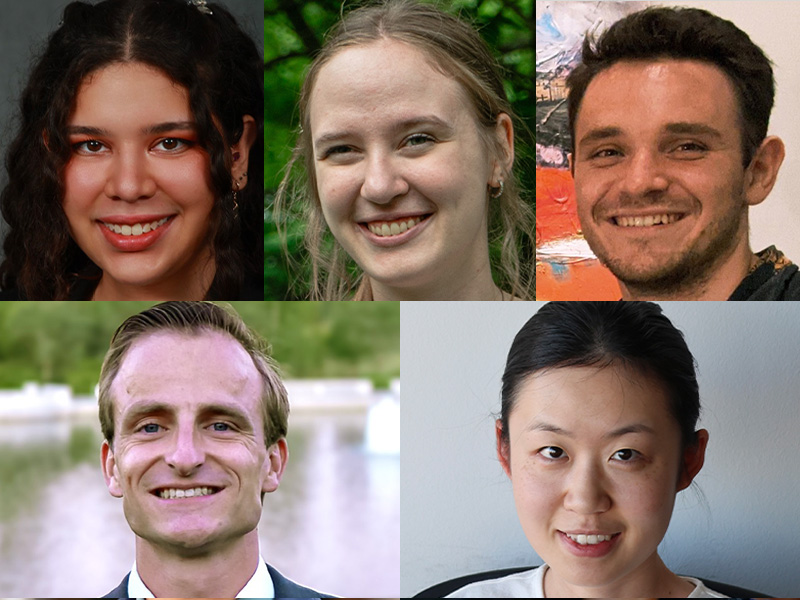
Li W, Xiao Z, Zhao J, Aono J, Pizzella S, Wen Z, Wang Y, Wang C, Chakrabartty S. A portable and a scalable multi-channel wireless recording system for wearable electromyometrial imaging. IEE Transactions of Biomedical Circuits and Systems, early online access May 19, 2023, DOI: 10.1109/TBCAS.2023.3278104.
This work was supported by grants from the Bill & Melinda Gates Foundation (INV-035476, and INV-037302) and by a grant from NIH/Eunice Kennedy Shriver National Institute of Child Health and Human Development (R01HD105905).