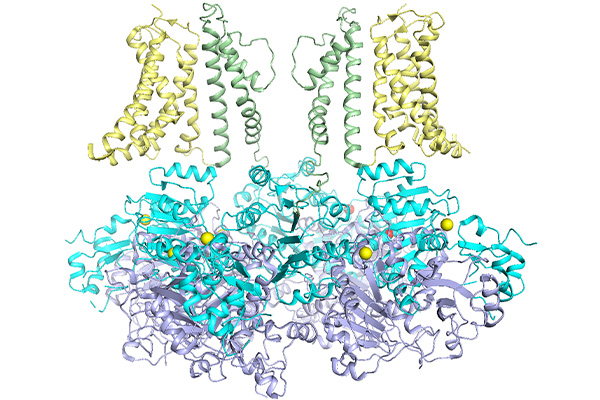
Genetic mutations in potassium ion channel target of new drug development
Jianmin Cui, collaborators to study potassium channelopathies and develop new drugs with NIH grant
Ion channels are involved in almost everything our body does, from regular heartbeats to muscle function to allowing communication within the body. When something goes awry in the ion channels, it can have devastating effects on the body.
Jianmin Cui, professor of biomedical engineering in the McKelvey School of Engineering at Washington University in St. Louis, plans to develop precision medicine for channelopathies in the KCNMA1 BK potassium ion channel with a five-year, $3 million grant from the National Institutes of Health’s National Institute of Neurological Disorders and Stroke. Cui’s collaborators include Huanghe Yang, associate professor of biochemistry, of neurobiology and of medicine at Duke University who earned master’s and doctoral degrees in biomedical engineering from WashU in 2007 and 2008, respectively; and Xiaoqin Zou, Curators’ Distinguished Professor at the University of Missouri.
Prior to 2005, researchers knew genetic mutations in potassium ion channels led to epilepsy and heart arrhythmias such as Long QT syndrome. In 2005, new research showed that mutations in a gene in the BK potassium ion channel led to a variety of severe neurodevelopmental disorders, cognitive impairments and movement disorders. These disorders manifest differently in nearly every patient, creating a challenge for caregivers and clinicians.
Since researchers found the first channelopathy in KCNMA1, more than 40 new variants associated with neurological disorders have been reported. And in the past year, researchers have found nearly 80 new variants. However, the mutations can occur in many different locations of the ion channel structure, causing a wide range of symptoms, from intellectual and developmental disabilities to ataxia and dystonia.
“Some of these mutations increase the channel activity,” Cui said. “These mutations will make the channel work better in certain circumstances. But some of them are loss of function, which have different symptoms, but can also overlap. We don’t know why the increase or loss of function would cause different symptoms and affect the cells and brain in different ways.”
With the federal funding, Cui and his collaborators plan to study how the mutations affect the molecular mechanism of BK channel activation to understand if the mutation affects the voltage-dependent activation, the calcium-dependent activation or another more intrinsic activation of the channel.
“We want to find those things to develop a strategy for different patients,” Cui said. “For example, if this channel is affected in intrinsic opening to cause certain diseases, then we try to use a strategy of drug screening that directly targets that intrinsic opening so that it can hopefully correct the symptoms for that particular kind of patient effectively without damaging the total function of the channel.”
Using electrophysiology, Cui’s lab will identify the molecular mechanisms of the channel and how the mutations change the channel function that lead to disease or disorder. The lab will also look to find the location of the mutation in the channel, which helps to pinpoint the exact target for potential drug development. Zou’s computational lab at the University of Missouri will perform docking, which places thousands of chemicals onto those locations of the ion channel identified by Cui’s lab to determine if one or more will bind there and ultimately change the channel function and the molecular mechanism. Yang’s lab at Duke will create mouse models of the channel mutations and test the compounds to determine their effectiveness on symptoms.
“There is no particular drug that is effective in treating this,” Cui said. “There are drugs that treat some of the symptoms, such as anti-seizure drugs, but we want to find a drug specific to the specific mutations to treat patients more effectively without a high dosage, which can often cause other problems.”
Cui and his collaborators are motivated in their work by the families and caregivers of those with these debilitating disorders.
“While these diseases are uncommon, for those affected, it’s very, very bad and just destroys the life of the patient, and to a certain extent, the family,” he said. “It is very important to try to find a cure. There may be a genetic component to this, and there may be drugs that could help. It’s a step in the right direction.”




