Common heart ailment target of new WashU Engineering research
Jon Silva and his team will study how small molecules and proteins interact with ion channels in the heart to cause and prevent arrhythmia, when the heart beats too fast, too slow, or is too unstable

More than 14 million Americans have an irregular heartbeat that predisposes them to sudden death. New research by a biomedical engineer at Washington University in St. Louis seeks to understand the issue at the molecular level with the goal of improving therapies.
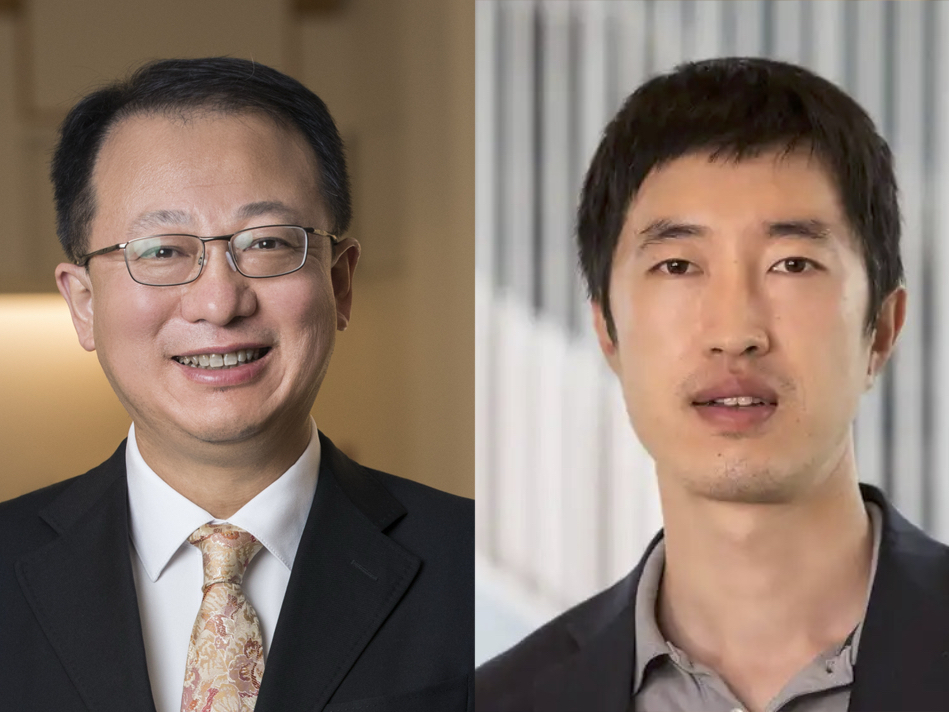
Jonathan Silva, assistant professor of biomedical engineering in the School of Engineering & Applied Science, will conduct the research with a five-year, $1.9 million grant from the National Heart, Lung, and Blood Institute of the National Institutes of Health. Specifically, Silva and his
team will study how small molecules and proteins interact with ion channels in the heart to cause and prevent arrhythmia, when the heart beats too fast, too slow, or is too unstable.
"When people are trying to treat arrhythmias, they are trying to control the behavior of the whole organ with a molecule," Silva said. "Unfortunately, when you take multiple molecular properties and put them together, you get a new behavior at the cell and tissue levels that's very hard to predict."
Silva will use a type of specialized molecular imaging called voltage-clamp fluorometry to watch how the ion channels move and to understand how drugs control the molecules, then create a computer model with the information.
"We've developed a system so we can look at four different parts of the channel and understand how all of them move," Silva said. "That's the information we'll put into our computer model. Then we can start to understand how those molecular motions affect the cells, how they affect the heart tissue, how they affect the whole organ, how those molecules can be therapeutically beneficial and maybe how we can improve them."
By understanding how the molecular level influences the cell tissue and heart levels, engineers and researchers can develop insight into better drugs. The drugs that Silva and his team will study are those that target the sodium channels, including lidocaine, a sodium-channel blocker.
"If we can understand how the drug affects the channel and then create a computational model to understand how that interaction affects the heartbeat, then we hope we can develop an improved therapy," he said.
This improved knowledge of activity at the molecular level would allow for specifically targeted drugs, Silva said.
"If a patient has atrial fibrillation, we want to use our molecule-level insight to get to get the drug to affect a specific target, the atrial cells, without affecting the ventricular cells," he said. "Right now, often people try to treat atrial fibrillation but cause ventricular fibrillation instead."
Silva and the members of his lab use immature egg cells called oocytes of the Xenopus, a clawed frog that is a model organism for development biology, as well as cardio myocytes derived from induced pluripotent stem cells, or stem cells generated from adult cells by reprogramming them.
"The oocytes allow us to isolate the one protein we want to look at and study it very carefully and very reproducibly, and that gives us great information about the mechanisms that we need to make a computer model," Silva said. "Then, we can take the computer model and compare it to the data we get from the induced pluripotent stem cells and see if our model predictions are correct."