Heart disease model puts cells to work
Researchers at Washington University in St. Louis can more effectively study mutations that cause heart disease by putting cells through their paces

Using animals to study heart disease doesn’t always translate well to human health outcomes, and human heart cells available for research don’t work outside the human body.
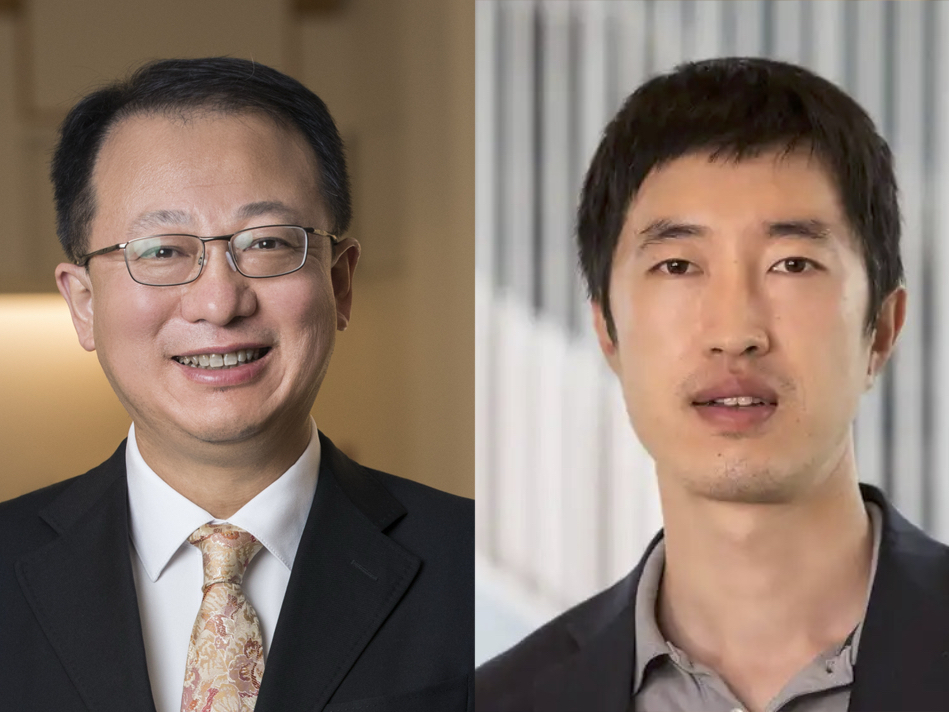
“You can’t keep them alive, much less function outside of the person for long enough to study these processes,” said Nathaniel Huebsch, an assistant professor of biomedical engineering in the McKelvey School of Engineering at Washington University in St. Louis. Huebsch is studying cells with a mutation that causes hypertrophic cardiomyopathy (HCM), a disease that can set off heart failure with little warning.
Huebsch and colleagues get around this challenge by tricking stem cells into behaving like mature heart cells, inducing pluripotent stem cell (iPSC)-derived cardiomyocytes to behave as if they are grownup heart cells bearing the mutation that causes HCM. They detail their findings in a paper recently published in iScience.
To make stem cells function like mature heart cells, scientists run the cells through a bootcamp of “mechanical stresses.” Essentially, they are trying to replicate the movement and resistance a heart cell experiences as being part of a moving muscle. If they attach their stem cells to a stiff interface, the cell has to “work” to pull on it. The work of a heart cell might also be key to how the mutation causes the disease.
Jonathan Silva, a professor of biomedical engineering at McKelvey Engineering and a co-author of the research, said that an electrical arrhythmia often affects people who have HCM, but the mutation is nowhere near the genes that encode for electrical activity.
The mutation is in the part of the genome that encodes for mechanics, squeezing proteins called sarcomeres. If there is something wrong in a movement protein, why does the electricity get affected?
“It’s like the lights go out even though you have a plumbing problem,” Silva said.
With this new research, Silva and Huebsch now have better idea of why this might be the case.
Huebsch said these myosin binding protein C (MYBPC3+/− ) mutations cause very subtle changes in the structure of the myofilament, the part of the cell that converts calcium into force. In HCM, it appears the mechanical stress mutation is affecting the way calcium is being shuttled into the cell so much so that it makes the cell prone to an arrhythmia event.
This research moves the field forward because connection between mechanical and electrical function in hearts isn’t well studied, and this work shows how genetic variance in mechanical proteins can cause electrical problems, Silva said.
Using computational tools, Silva hopes to find which specific calcium channels are being disrupted, tinker with drugs, mechanical stresses and model different ways to predict outcomes in patients.
J Guo, H Jiang, D Schuftan, JD Moreno, G Ramahdita, L Aryan, D Bhagavan, J Silva, N Huebsch. Substrate mechanics unveil early structural and functional pathology in iPSC micro-tissue models of hypertrophic cardiomyopathy. iScience. 2024 May 0;27(6):109954. DOI: https://doi.org/10.1016/j.isci.2024.109954
This work was supported by the American Heart Association (19CDA34730016 to N.H., predoctoral fellowship 828938 to J.G., TPA 970198 to N.H.), the Center for Engineering Mechanobiology—National Science Foundation Science & Technology Center CMMI No. 15-48571 (G.R.), and the National Institutes of Health (R01 HL159094 to N.H.)